|
Spondylolisthesis
Claudio Lamartina
Introduction
Spondylolisthesis is a word of Greek origin: spondylos means vertebra and olisthesis slippage. It defines
the anterior slippage of a vertebra on to the one below. The lumbasacral junction is the most common
region involved, followed by middle lumbar spine, cervical spine and, exceptionally, thoracic spine. The
incidence in childhood is 4%, while in adulthood it becomes 4-6%. It has been noted that genetic factors
play a major part in spondylolisthesis. In fact, a 50% incidence was found in some Eskimo groups.
Since spondylolisthesis can be asymptomatic, it can often remain undetected. If symptomatic, it can
cause back and/or leg pain, neurologic deficit and progressive deformity, and therefore requires
treatment. The treatment can be non-surgical, although in given cases surgery is indicated.
Among spondylolisthesis there is a variety of different forms of anterior-slippage of a vertebra. These
various forms have different biomechanics and different evolution and therefore require different
treatments. For this reason classification is extremely useful.
Classification
The Wiltse classification [11] is the one which is most widely used.
Wiltse classification of spondylolisthesis:
I) Congenital:
- Dysplastic posterior elements and articular processes, often associated with spina bifida.
- Dysplastic articular processes with sagittal orientation of the facet joints giving instability at
L5-S1.
- C. Other congenital anomalies, e.g. congenital kyphosis, which causes slippage.
II) Isthmic:
- Lytic, probably a stress fracture of the pars interarticularis.
- Elongated with intact pars interarticularis, presumed to be a healed type IIA.
III) Degenerative
IV) Post-traumatic: acute fracture and⁄or ligamentous injury in a different area from the pars
interarticularis.
V) Pathologic: bone disease that produces degeneration of articular processes resulting in
Spondylolisthesis.
VI) Post-surgical: result of loss of posterior elements due to surgery.
The Wiltse classification has the disadvantage of placing together anatomic and etiologic factors, and it
is not always easy to distinguish type I from type II. Besides, his precise classification may be
irrelevant.
The Marchetti-Bartolozzi classification [7] overcomes this disadvantage as it is etiologic and easier to
use.
Marchetti-Bartolozzi Classification of spondylolisthesis:
I) Developmental
- High dysplastic with lysis or with elongation.
- Low dysplastic with lysis or with elongation.
II) Acquired
- Traumatic, which is due to acute or stress fracture.
- Post-surgery, which is caused by direct or indirect surgery.
- Pathologic, which is due to local or systemic pathology.
- Degenerative, found in primary or secondary degenerative conditions.
High dysplastic developmental spondylolisthesis is characterized by pelvic retroversion with
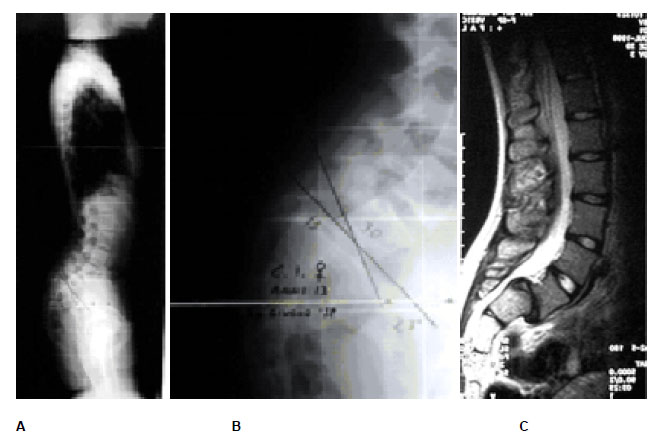
verticalisation of the sacrum and anterior displacement of the centre of rotation of the hip joints (fig. 1).
Fig. 1 The sagittal profile with hyperlordosis of a 13-year-old girl with high dysplastic developmental spondylolisthesis (A). The anterior displacement of the hips and the verticalisation of the sacrum are the result of pelvic retroversion (B, C).
Low dysplastic developmental spondylolisthesis has an almost normal bony anatomy with slippage that rarely becomes severe (fig. 2).
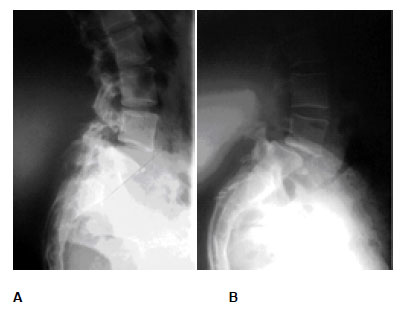
Fig. 2 The 18-year evolution of low dysplastic developmental spondylolisthesis in a 40-year-old woman; at 22 years of age (A) and at 40 years (B).
Acquired types of spondylolisthesis are caused by traumatic, post-surgery, pathologic and degenerative conditions (fig. 3).

Fig. 3 A 17-year-old male road accident victim. X-rays taken at the time of the accident (A, B). Severe slippage after 2 months of conservative treatment (C). Posterior surgery was performed with reduction, instrumentation and fusion (D).
Marchetti and Bartolozzi suggest that the two types of dysplastic developmental spondylolisthesis are only different morphological expressions of the same etiologic process. However, if we observe carefully an x-ray of low dysplastic type and an x-ray of high dysplastic type there are remarkable differences, not only morphological but also biomechanical (fig 4).
Fig. 4 X-ray showing a low dysplastic developmental spondylolisthesis where, apart from the lysis with slippage and degenerative changes, the bony anatomy is almost normal (A). X-ray showing a high dysplastic form, where the bony anatomy is abnormal, with a vertically displaced sacrum and a rounded dome (B).
Biomechanics
Vidal and Marnay [10] studied the sagittal alignment in both normal subjects and in patients with
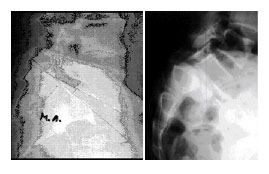
spondylolisthesis. In normal subjects, the gravity line from the external auditory meatus falls across L5-S1 and passes through the centre of the femoral head; it is continuous. Sometimes, even in normal subjects, this alignment is lost at the L5-S1 level due to a slight anterior displacement of the hips, and in this event a minor torque (two opposing forces which produce rotation) is created. In patients with high dysplastic developmental spondylolisthesis, the alignment is always lost and the torque is of much greater force (fig. 5).
Fig 5 Standing x-ray showing a normal alignment (A). Standing x-ray in high dysplastic developmental spondylolisthesis showing a major shift of the spine and trunk (B). For measurements see text.
Vidal and Marnay defined this torque as couple charnière. It is composed of the body weight (whose force application point is on L5-S1) and of the ground reaction transmitted through the hips (whose force application point is at the centre of the femoral head). They calculated that the percentage (hereafter called C) between the horizontal segment from the centre of S2 to the point of intersection with the vertical line coming from the external auditory meatus (D1 in fig 5), and the segment going from the centre of S2 to the intersection with the vertical line which starts from the ground and passes through the centre of the femoral head (D2 in fig 5), is more than 80% in a normal subject (fig 5 A).
In spondylolisthesis the more slippage, pelvic retroversion, verticalisation of the sacrum and anterior displacement of the hips is present, the larger the torque and the lower C become (fig 5 B). Pelvic retroversion is the cause and effect of both the anterior displacement of the hips and the verticalisation of the sacrum. Pelvic retroversion influences slippage and causes the loss of normal trunk alignment along the line from the external auditory meatus, lumbar sacral joint and centre of femoral head (gravity line). These factors determine the evolution of each case.
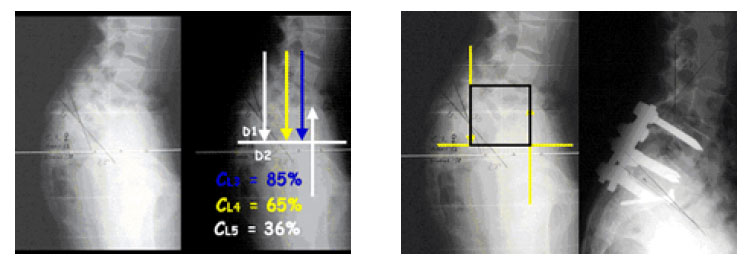
Applying the study of Vidal and Marnay, it is possible to state that the unstable zone (fig. 6 B) in a high displastic developmental spondylolisthesis always includes the slipped L5 and sometimes also L4 (theoretically also L3), if C is less than 80% on L4 due to high pelvic retroversion [6].
Fig. 6 Standing lateral x-ray showing a high dysplastic developmental spondylolisthesis (A), with C
calculated in L5, L4 and L3 (B). The unstable area includes the slipped L5, and L4 since its C is 65%, while L3 is excluded because C is more than 80%. The square indicating the unstable zone in this specific case includes L5 and L4 (C). Post-op x-ray showing the results with complete reduction of the L5 slippage and the inclusion of L4 in the instrumentation and fusion (D).
Severity Index
The traditional method to quantify the severity of slippage is based on the system of Meyerding [8]
which is widely used in all cases of spondylolisthesis. This method cannot be applied to high dysplastic developmental spondylolisthesis because, as shown above, the iomechanics is completely different from all other forms. In the former more slippage does not necessarily correspond to higher severity. The amount of pelvic retroversion with verticalisation of the sacrum and anterior displacement of the hips, can be a more precise factor in evaluating the severity, because the pelvic retroversion, and not the percentage of slippage, defines the amount of L5-S1 torque as described by Vidal and Marnay.
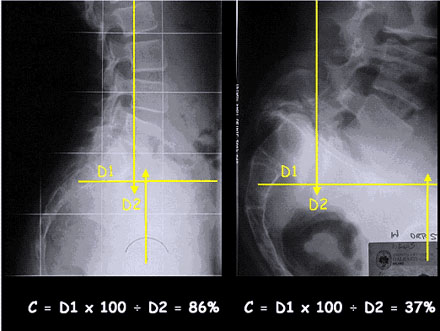
Obviously, with equal percentage of slippage, more pelvic retroversion defines higher severity, and vice versa. However, of the two, the pelvic retroversion is more important, since this produces the slippage and not vice versa (fig. 7 A and B).
This means that low C indicates higher severity.
Fig. 7 In x-ray A the spondylolisthesis with 50% slippage and C 36% has greater pelvic retroversion than in x-ray B with 65% slippage and C 67%. X-rays C and D are the same X-rays as in A and B. We can observe the different way of calculating SI with respect to C.
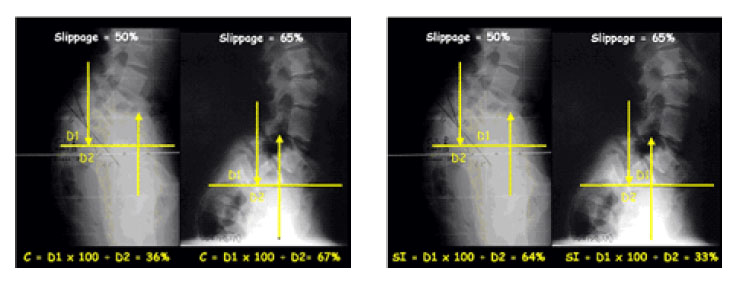
More recently, Farcy and Schwab [4] described a sagittal pelvic tilt index which, like the Vidal and
Marnay Index C, is indirectly proportionate to the pelvic retroversion and for this reason less useful in evaluating the severity of high displastic developmental spondylolisthesis. A directly proportionate measurement would be better. Like the calculation of Vidal and Marnay’s C, in a lumbosacral lateral standing x-ray including the hips (fig. 7 C and D), a horizontal line can be drawn from the centre of S2, intersects a vertical line coming from the centre of L5-S1 and another vertical line from the centre of the hips. But different from Vidal and Marnay’s Index C, we can calculate the value of the Severity Index (SI) in spondylolisthesis in this way:
SI = D1 x 100 ÷ D2.
SI is a direct measurement of the pelvic retroversion, since the higher D1 is, the greater the anterior displacement of the hips is. For this reason this value is directly proportionate to the severity of the spondylolisthesis.
Reduction
Case presentation 1 (fig. 8)
Thirty year old woman with back and leg pain for more than 1 year; conservative treatment was carried out without success. At clinical examination a bilateral L5 strength deficit was found. In order to investigate the patient an X-ray and an MRI were done. Since the pain was progressive and there was a root deficit, surgery was indicated. Posterior reduction with instrumentation and ALIF was performed with complete relief of the symptoms.
Fig. 8 X-ray showing the square which demonstrates that the unstable area includes only L5; slippage = 61%, SI = 34% (A). X-ray showing better L5-S1 (B). MRI showing the sacrum ysplasia with S1-S2 kyphosis ( C). X-ray showing at one-year follow-up a posterior instrumentation and anterior cage with a circumferential fusion. The reduction is stable and implants are in place (D).
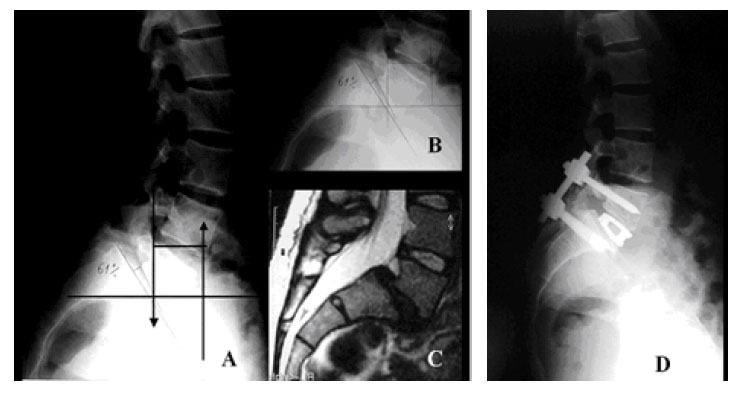
Rationales of treatment in adult
Indication for surgery on an adult with high dysplastic spondylolisthesis comes from the persistence of symptoms, including neurological, resistant to conservative treatment. The evaluation of the unstable area by means of drawing the square indicates the fusion area if a reduction is planned [6]. In the case of in situ fusion, the fusion area must also include the L4-L5 disc only if it is symptomatic (evocative discography). The SI allows us to evaluate the severity of the spondilolisthesis independently of the slippage.
Rationales for reduction in Case 1 were:
- L5 deficit which requires decompression (the best decompression is reduction)
- largest possible fusion area (severe slippage)
- chance to obtain normal anatomy since the sacrum dysplasia is slight (low SI=36%, only S1-S2 kyphosis)
- prevent early degenerative changes in L4-L5 disc
- greatly reduced fusion area (only L5 as seen in the square)
Although neurological risks do exist [1,2,3,5,9], the reduction of spondylolisthesis allows for the best decompression, the best fusion area and for a normal anatomic alignment of the pelvis and trunk.
However, when a reduction has been performed, a circumferential fusion is mandatory, because without interbody fusion (ALIF or PLIF) either the reduction can be lost or the instrumentation can fail (fig. 9).
Fig. 9 X-ray showing a low dysplastic developmental spondylolisthesis (A). X-ray at the four-month
follow-up showing a reduction performed with posterior instrumentation only, and postero-lateral
fusion, without PLIF or ALIF for the slight slippage. We can see that one sacral screw is broken, due to the lack of interbody fusion (B).

Case presentation 2 (fig. 10)
Fourteen year old girl with severe back pain for 1 year. Conservative treatment was carried out without success. At clinical examination no neurological deficits were found. In order to investigate the patient an X-ray and an MRI were done. The Risser sign was 1 and the discs above L5 were normal. Since the pain was progressive and there was a great risk of progression, surgery was indicated. As the girl was extremely thin, a posterior reduction with internal fixator was impossible because of its excessive volume under the skin. After posterior intraoperative reduction levering between L5 transverse processes and sacral wings, two L5-S1 pediculo-body screws were inserted posteriorly and an anterior interbody fusion with anterior screw and autogenous bone grafting was performed with complete relief of the symptoms.
Fig. 10 X-ray showing the square which demonstrates that the unstable area includes only L5;
Slippage = 50%, but with high SI = 53% (A). X-ray showing better L5-S1 (B). MRI showing the severe sacrum dysplasia with its verticalization (C). X-ray showing at one-year follow-up posterior pediculobody screws and anterior interbody screw. The reduction is stable and the screws are in place (D).
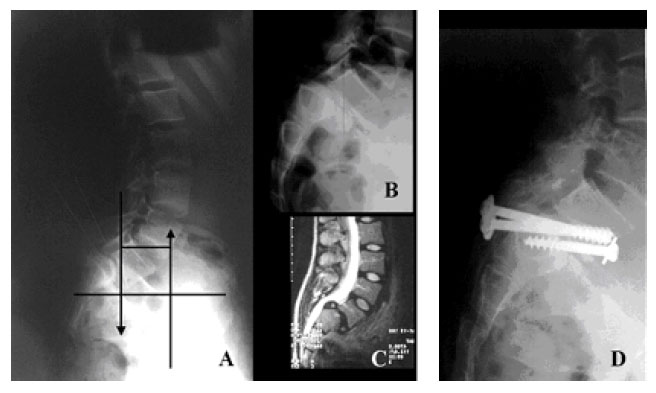
Rationales of treatment in adolescent
Indication for surgery on an adolescent with high dysplastic spondylolisthesis comes from the presence of symptoms, including neurological, and from the risk of progression. The evaluation of the unstable area by means of drawing the square indicates the fusion area if a reduction is planned [6]. In the case of in situ fusion, the fusion area must, exceptionally, include the L4-L5 disc (evocative discography). The SI allows us to evaluate the severity of the spondylolisthesis independently of the slippage (fig. 11).
Rationales for reduction in Case 2 were:
- high SI (risk of postop decompensation)
- largest possible fusion area (severe slippage)
- chance to obtain normal anatomy due to the young age
- prevent early degenerative changes in L4-L5 disc
- greatly reduced fusion area (only L5 as seen in the square)
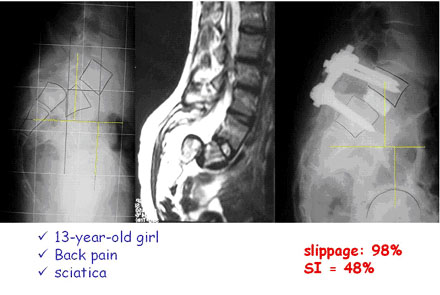
Fig. 11 X-ray showing the square which demonstrates that the unstable area includes only L5; Slippage = 98%, with high SI = 48%. MRI showing the severe sacrum dysplasia with its verticalization. X-ray showing at one-year follow-up that the reduction is stable; the patient is pain free.
Since there are no clear answers in literature, studies should be carried out to see how to prevent root damage during the reduction manoeuvres, and to evaluate the results on the symptoms of reduction vs in-situ fusion.
References
1. Ani N, Keppler L, Biscup RS, Steffe AD (1991) Reduction of high-grade slips (grade III-IV) with VSP instrumentation, report of a series of 41 cases. Spine 16:S302-S310
2. Boos N, Marchesi D, Zuber K, Aebi M (1993) Treatment of severe spondylolisthesis by reduction and pedicular fixation: a four to six year follow-up study. Spine 18:1655-1661
3. Dick W, Schnebel B (1988) Severe spondylolisthesis: reduction and internal fixation. Clin Orthop
232:70-79
4. Farcy J-P, Schwab FJ (1997) Management of flatback and related kyphotic decompensation
syndromes Spine 20(22):2452-2457
5. Hu SS, Bradford DS, Transfeldt EE, Cohen M (1996) Reduction of high-grade spondylolisthesis using Edwards instrumentation. Spine 21:367-371
6. Lamartina C (2001) A square to indicate the unstable zone in severe spondylolisthesis. Eur Spine J 10:444-448
7. Marchetti PG, Bartolozzi P (1986) Spondylolisthesis – Classification and etiopathogenesis. Progress in spinal pathology: Spondylolisthesis II. Bologna, Italy: Italian Scoliosis Research Group
8. Meyerding HW (1932) Spondylolisthesis. Surg Gynecol Obstet 54:371-377
9. Molinari RW, Bridwell KH, Lenke LG, Ungacta FF, Riew KD (1999) Complications in the surgical treatment of pediatric high-grade isthimic spondylolisthesis : a comparison of three surgical approaches. Spine 24:1701-1711
10. Vidal J, Marnay T (1983) La morphologie et l’équilibre corporel antéro-postérieur dans le
spondylolisthèsis L5-S1. Rev Chir Orthop 69:17-28
11. Wiltse LL, Newman PH, MacNab I (1976) Classification of spondylolisis and spondylolisthesis. Clin Orthop 117:23-29
|